Whether you are heading towards your twenties, you are already in your twenties, or you have passed your twenties a long time ago: taking care of and understanding your reproductive health is important! Your twenties are often called the formative years. For many of us, this phase is about the transition from college to work life, leaving the parental house, and exploring the world, others, and ourselves. We think of ourselves as being young, wild, and free! Your twenties are also filled with many people who confirm this idea. Oh, you are still young and have a whole life ahead of you, enjoy your time, do not think of having children yet. And this is also reflected in how many of us think of our reproductive health during this phase: contraception. In this blog post, I will focus on the things that you should know about your reproductive health during this phase.
Fertility
This might not come as a surprise as lately a lot has been published about the female “biological clock”, but according to research, your twenties are your most reproductive years. Studies reveal that women aged 20-24 have a slightly higher chance of getting pregnant compared to women aged 25-29.[1] No need for panic, if you belong to the latter group and want to have children, overall if you are in your twenties you are the most fertile. Does this mean that women who are in their twenties cannot have fertility issues? No. Fertility issues can have multiple causes, but the main reason is the inability to ovulate and this can happen at any age.[2] If you are in your twenties and you know that you want to have children later in life or you have not decided yet, it can be a good idea to observe your menstrual cycle to check whether there might be any fertility issues. Irregular menstruation cycles might be a sign of irregular ovulation or no ovulation. I have also read that you can keep an eye on hormonal changes or that women take a blood test to check their levels of follicle-stimulating hormone. I am by no means a gynaecologist or a GP though and I have no idea whether you can get tested easily. So, if you have concerns about your fertility, I recommend visiting your GP.
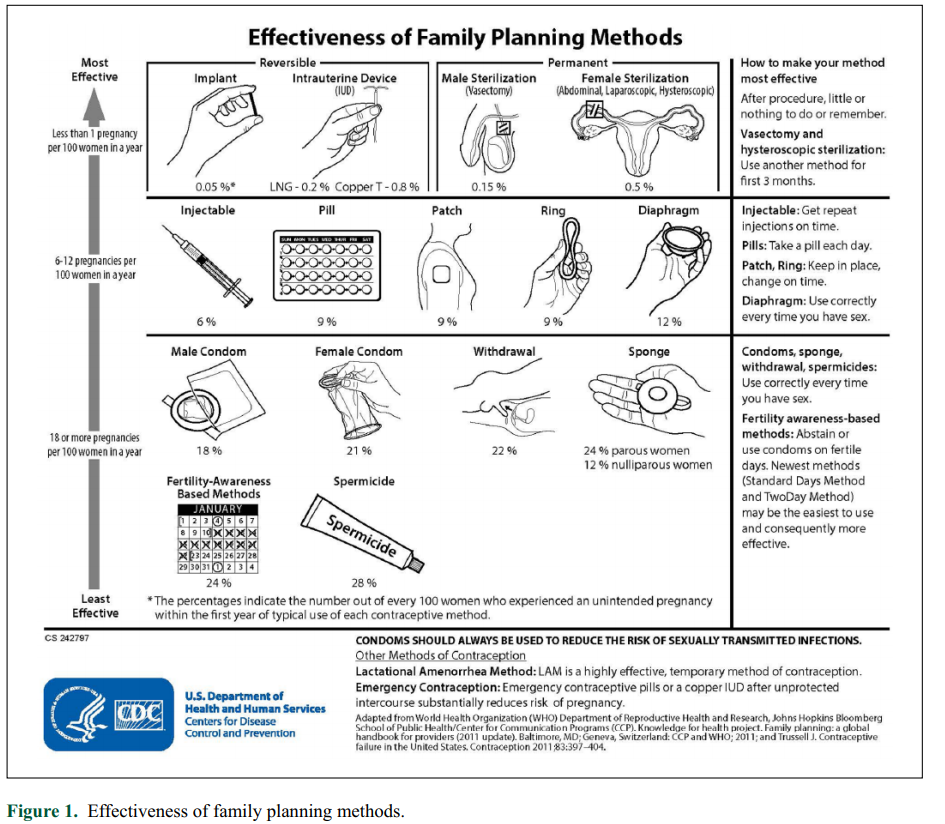
Contraception
Every woman’s body is different, and women have different preferences for various contraceptive methods. Many elements need to be considered when choosing the appropriate contraceptive methods. These elements include safety, effectiveness, availability, affordability, and acceptability. There are 15 methods of contraception and recently all eyes are on a new one: the male pill. Researchers and experts are still testing this, so it might take a while for this one to enter the market. When we look at the methods that are used now, we can make a distinction between permanent and non-permanent methods and hormonal and non-hormonal methods. I will discuss the methods from most effective to least effective (see figure 1).[3] Permanent methods include female and male sterilization, and these are also the most effective (less than 1 pregnancy per 100 women). There are also the reversible methods (implant and intrauterine device), also called “emergency contraception”, these can be used when you did not use any protection but still want to prevent a pregnancy. Now we move the less effective methods and non-permanent methods (6-12 pregnancies per 100 women). These are the injectable, pill, patch, ring, and diaphragm of which all except for the diaphragm are hormonal methods. The least effective (18 or more pregnancies per 100 women) are the condoms, withdrawal, sponge, fertility-awareness based methods, and spermicide. All of these except for the fertility-awareness based method are also called barrier methods, because they block the sperm from getting into the woman’s body.
There is a lot of criticism on the hormonal methods, because of the side effects. I have also read that women who have had the copper or mirena intrauterine device inserted, experience cramping and contractions. As said before, every woman’s body is different and reacts differently to the methods, and it is up to you and your partner to decide which contraceptive methods work the best for the both of you and feel pleasant.
Sexually transmitted infections (STIs)
Just when you think “phew, I know what contraceptive methods I want to use to prevent pregnancy” … It is important to keep in mind that contraception is also necessary to prevent getting infected. Examples of STIs are chlamydia, gonorrhoea, HIV, hepatitis B, herpes genitalis, syphilis, trichomoniasis, human papillomavirus (HPV), herpes simplex virus (HSV).[4] There are 4 curable diseases: syphilis, gonorrhoea, chlamydia and trichomoniasis. The diseases that are not curable are: hepatitis B, HSV or herpes, HIV, and HPV. The danger lies in that many of these diseases do not have symptoms or signs. In the case of chlamydia and gonorrhoea, people not always experience pain, while the consequences are huge, because you can get infertile. STIs can be prevented by contraceptives, such as condoms. You should get tested when you have symptoms, such as pain around the pubic area, discharge, blisters, or warts.
If you have questions or concerns about your reproductive health, talk with your doctor. I am also seeing discussions on sexual issues in women’s groups on social media. It might a good idea to join those groups and read about the experiences of other women or ask your question anonymously if you feel uncomfortable. You will notice that many women struggle with the same issues and there is nothing to be uncomfortable about. Recognize your needs and feel comfortable with your choices.
[1] Garcia, D., Brazal, S., Rodriguez, A., Prat, A., & Vassena, R. (2018). Knowledge of age-related fertility decline in women: a systematic review. European Journal of Obstetrics & Gynecology and Reproductive Biology, 230, 109-118.
[2] Brugo-Olmedo, S., Chillik, C., & Kopelman, S. (2001). Definition and causes of infertility. Reproductive biomedicine online, 2(1), 173-185.
[3] Houtchens, M. K., Zapata, L. B., Curtis, K. M., & Whiteman, M. K. (2017). Contraception for women with multiple sclerosis: Guidance for healthcare providers. Multiple Sclerosis Journal, 23(6), 757–764. https://doi.org/10.1177/1352458517701314
[4] World Health Organization (2019). Sexually Transmitted Infections.